If you are enrolled in Medicare, you might not need to do anything for a renewal of your Medicare coverage. In many cases, your Medicare coverage will automatically renew each year.
There may be some situations, however, in which your Medicare coverage will not renew.
You may also want to review your Medicare coverage each fall to take advantage of other Medicare plan options that could potentially offer you more coverage and save you money.
Compare plans today.
Speak with a licensed insurance agent
Will my Medicare Part A and/or Part B plan automatically renew?
If you have Medicare Part A (hospital insurance) and/or Part B (medical insurance) and you are up to date on your Medicare premiums, your Medicare coverage will automatically carry over from one year to the next and there is nothing you need to do to renew your plan.
Will my Medicare Advantage plan auto-renew?
If you have another form of Medicare coverage – such as a Medicare Advantage plan (Medicare Part C), a Medicare Part D plan or a Medicare Supplement Insurance plan (Medigap) – your coverage should renew automatically, as long as the plan is still being provided and you are paying your plan premiums.
When will my Medicare plan not automatically renew?
Situations in which these types of Medicare plans might no longer be provided can include:
- The plan is deemed to be low performing
Medicare rates all Medicare Advantage plans and Part D plans each year using the Medicare Star Rating system. Each plan is given a rating of one to five stars, with five stars being the highest ranking.2
If a plan receives fewer than three stars for three consecutive years, Medicare will flag the plan as low performing. Medicare reserves the right to discontinue low-performing plans from being offered.
If this happens, all members of the plan will receive a notice informing them of the decision, and they will be granted a Special Enrollment Period to sign up for a different Medicare plan.
- The plan stops serving your area
A Medicare Advantage plan, a Part D plan or a Medicare Supplement Insurance plan may occasionally change its coverage area and stop providing benefits to a particular location.
If this happens, plan members may be given a Special Enrollment Period to sign up for a different Medicare plan that is offered in their area for the coming year.
- The insurance company stops providing the plan
Medicare Advantage plans, Medicare Part D plans and Medicare Supplement Insurance plans are sold by private insurance companies. The company that provides a plan may choose to no longer offer that specific plan.
If this happens, plan members may be granted a Special Enrollment Period to enroll in a new Medicare plan.
Review your Plan Annual Notice of Change (ANOC)
If you’re enrolled in a Medicare Advantage plan or a Medicare Part D plan, you will receive a “Plan Annual Notice of Change” in the mail each September.
This notice will call attention to any changes in plan costs, benefits or service area adjustments for the upcoming year.
If there are any changes made to your plan that affect your overall satisfaction with the coverage, you may have a few opportunities to make any desired changes.
When can you make changes to your Medicare coverage?
There are a few times throughout the year that you may be able to make changes to your Medicare coverage, including Medicare Advantage and Medicare Part D prescription drug plans.
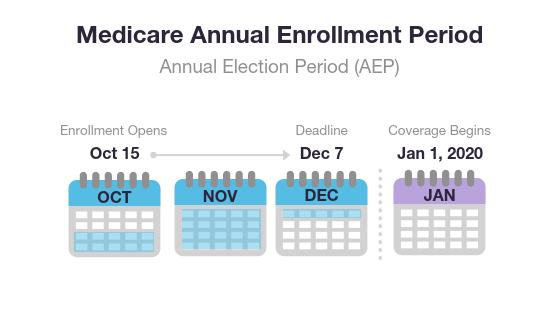
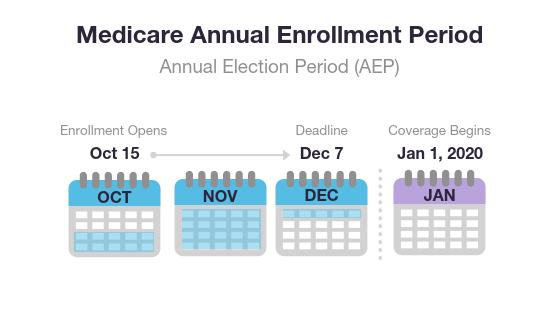
The Annual Enrollment Period (AEP)
The Medicare Annual Enrollment Period (also known as the Fall Medicare Open Enrollment Period for Medicare Advantage plans) takes place each year from October 15 to December 7.
During this time, you may join, leave or switch Medicare Advantage plans or Medicare Part D plans.
The Five-Star Medicare Enrollment Period
Anyone who is enrolled in a Medicare Advantage or Medicare Part D plan with a rating of fewer than five stars is typically eligible to make changes to their Medicare coverage during the Five-Star Special Enrollment Period.2
From December 8 to November 30 of the following year, you may change your Medicare coverage in the following ways:
- Switch from Original Medicare to a five-star Medicare Advantage plan
- Switch from a Medicare Advantage plan with fewer than five stars to a five-star plan
- Switch from a Part D plan with fewer than five stars to a five-star plan
- Switch from one five-star Medicare Advantage plan to another five-star Medicare Advantage plan
- Switch from a Medicare Advantage or Part D plan to a five-star Medicare Cost Plan
Medicare Special Enrollment Period (SEP)
Some Medicare beneficiaries may qualify for a Special Enrollment Period (SEP) at any time throughout the year to beneficiaries who experience a qualifying event.
These can include (but are not limited to):
- Moving out of your plan’s service area or moving to an area with additional coverage options
- Moving back to the U.S. after living outside of the country
- Residing in, moving into or moving out of a skilled nursing facility or long-term care hospital
- Being released from jail
- Losing Medicaid eligibility
- Losing or leaving employer, union or COBRA coverage
- Losing drug coverage that’s at least as good as Medicare drug coverage
- Medicare terminates its contract with your plan or takes a sanction against it
There are other reasons a beneficiary may qualify for a Medicare SEP. A licensed insurance agent can help you determine your eligibility.
Medicare General Enrollment Period (GEP)
The Medicare General Enrollment Period (GEP) lasts from January 1 to March 31 each year.
Beneficiaries who did not sign up for Medicare Part A or Part B during their Initial Enrollment Period may do so during the General Enrollment Period. However, you may be subject to late enrollment fees for doing so.
Will my Medicare Supplement (Medigap) plan auto-renew?
You may drop a Medicare Supplement Insurance plan at any time. However, you may have trouble being accepted into a new Medigap plan, and you will likely be subject to medical underwriting if you do so.
In many cases, you may be able to take advantage of a 30-day “free look” period:
- For 30 days, you can carry two Medigap plans: your current plan and the plan you are considering changing to.
- At the end of the 30 day period, you will decide which plan to keep and which one to drop.
- You will need to pay the plan premiums for both plans while you are enrolled in each plan.
Review your Medicare options each year
There are limited times throughout the year that you may drop, switch or add Medicare coverage, so it’s important to take advantage of those opportunities to review your coverage options instead of depending on automatic Medicare renewal.
Each fall, it’s wise to review your Medicare coverage and consider all of the following:
- Have any of your plan costs gone up?
- Have your plan benefits changed?
- Has the network of participating doctors changed? And more specifically, is your favorite doctor still part of your plan network?
- Have you experienced any changes in your health that require a different set of health insurance coverage?
- Will you be traveling outside the U.S. in the upcoming year?
- Will you be moving to a new address?
Get help with Medicare renewal and review plan options in your area
Fortunately, there’s an easy way to conduct your annual Medicare review. You can speak to a licensed insurance agent, who can help you review your Medicare benefits and any upcoming plan changes.
They can also help you compare other plan options available in your area and find plans that could potentially help you save money.
Or call 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent. We accept calls 24/7!